Research (Holtappels Laboratory)
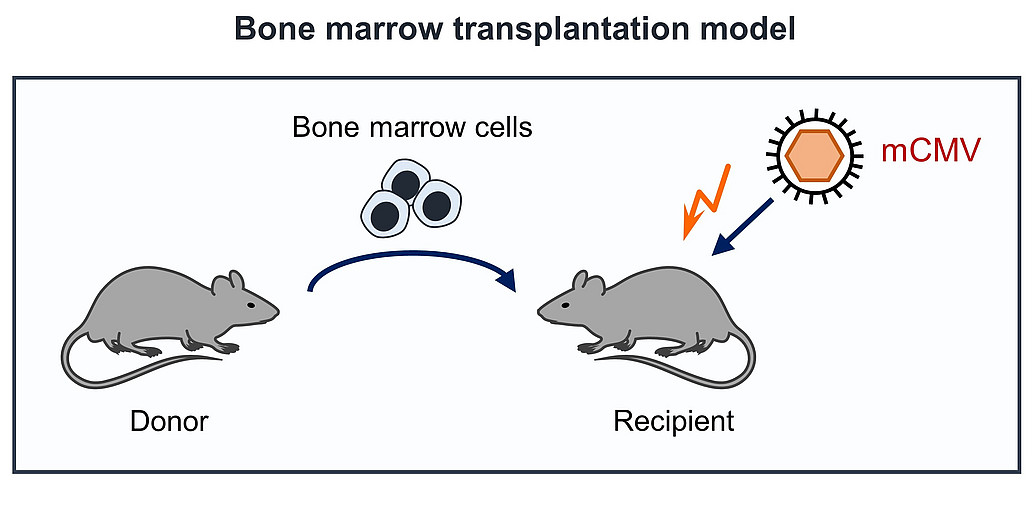
The major research topic of our group is the study of the immune control of cytomegalovirus (CMV) infection in a mouse model. Control of CMV infection is dominated by CD8 T cells which are able to control the infection, but which are not able to clear the virus from the infected host. Our work aims at understanding this highly balanced virus host relationship under different immunological conditions.In particular, after bone marrow transplantation (BMT), primary or recurrent CMV infections imperil the survival of the transplant recipients. To understand the underlying mechanisms we established an experimental murine BMT model, in which a concurrent infection with murine CMV (mCMV) is eventually controlled by endogenously reconstituted CD8 T cells preventing lethal multiple organ disease [Holtappels et al., 2004; 2013; 2016; Ebert et al., 2014; Nauerth et al., 2013]. The immune response, however, is not efficient in precluding morbidity and in clearance of the viral genome. This bears the risk of productive virus reactivation under immunocompromising conditions.
Research topics
- Immune control of mCMV infection after experimental bone marrow transplantation (BMT).
- Significance of immunodominant CD8 T-cell specificities for the immune control of mCMV infection.
- Significance of the avidity of CD8 T cells with respect to their protective potential.
- Significance of vRAPs (viral Regulators of Antigen Presentation) on peptide presentation, T-cell priming, and immune control.
- Influence of CMV in the development of allergic airway disease [Reuter et al., 2019].
References
-
Holtappels R, Becker S, Hamdan S, Freitag K, Podlech J, Lemmermann NA, Reddehase MJ. Immunotherapy of cytomegalovirus infection by low-dose adoptive transfer of antiviral CD8 T cells relies on substantial post-transfer expansion of central memory cells but not effector-memory cells. PLoS Pathog. 2023. 19:e1011643. doi: 10.1371/journal.ppat.1011643.
Hamdan S, Reddehase MJ, Holtappels R. Cytomegalovirus immune evasion sets the functional avidity threshold for protection by CD8 T cells. Med Microbiol Immunol. 2023. 212:153-163. doi: 10.1007/s00430-022-00733-w.
Holtappels R, Podlech J, Freitag K, Lemmermann NA, Reddehase MJ. Memory CD8 T cells protect against cytomegalovirus disease by formation of nodular inflammatory foci preventing intra-tissue virus spread. Viruses. 2022.14:1145. doi: 10.3390/v14061145.
Freitag K, Hamdan S, Reddehase MJ, Holtappels R. Immunodominant cytomegalovirus epitopes suppress subdominant epitopes in the generation of high-avidity CD8 T cells. Pathogens. 2021. 10:956. doi: 10.3390/pathogens10080956.
Gergely KM, Podlech J, Becker S, Freitag K, Krauter S, Büscher N, Holtappels R, Plachter B, Reddehase MJ, Lemmermann NAW. Therapeutic vaccination of hematopoietic cell transplantation recipients improves protective CD8 T-cell immunotherapy of cytomegalovirus infection. Front Immunol. 2021. 12:694588. doi: 10.3389/fimmu.2021.694588.
Reddehase MJ, Holtappels R, Lemmermann NAW. Consequence of histoincompatibility beyond GvH-reaction in cytomegalovirus disease associated with allogeneic hematopoietic cell transplantation: change of paradigm. Viruses. 2021. 13:1530. doi: 10.3390/v13081530.
Holtappels R, Freitag K, Renzaho A, Becker S, Lemmermann NAW, Reddehase MJ. Revisiting CD8 T-cell 'Memory Inflation': New insights with implications for cytomegaloviruses as vaccine vectors. Vaccines (Basel). 2020. 8:402. doi: 10.3390/vaccines8030402.
Holtappels R, Schader SI, Oettel O, Podlech J, Seckert CK, Reddehase MJ, Lemmermann NAW. Insufficient antigen presentation due to viral immune evasion explains lethal cytomegalovirus organ disease after allogeneic hematopoietic cell transplantation. Front Cell Infect Microbiol. 2020. 10:157. doi: 10.3389/fcimb.2020.00157.
Reuter S, Lemmermann NAW, Maxeiner J, Podlech J, Beckert H, Freitag K, Teschner D, Ries F, Taube C, Buhl R, Reddehase MJ, Holtappels R. Coincident airway exposure to low-potency allergen and cytomegalovirus sensitizes for allergic airway disease by viral activation of migratory dendritic cells. PLoS Pathog. 2019. 15:e1007595. doi: 10.1371/journal.ppat.1007595.
Dekhtiarenko I, Ratts RB, Blatnik R, Lee LN, Fischer S, Borkner L, Oduro JD, Marandu TF, Hoppe S, Ruzsics Z, Sonnemann JK, Mansouri M, Meyer C, Lemmermann NA, Holtappels R, Arens R, Klenerman P, Früh K, Reddehase MJ, Riemer AB, Cicin-Sain L. Peptide processing is critical for T-cell memory inflation and may be optimized to improve immune protection by CMV-based vaccine vectors. PLoS Pathog. 2016. 12:e1006072. doi: 10.1371/journal.ppat.1006072.
Nauerth M, Weißbrich B, Knall R, Franz T, Dössinger G, Bet J, Paszkiewicz PJ, Pfeifer L, Bunse M, Uckert W, Holtappels R, Gillert-Marien D, Neuenhahn M, Krackhardt A, Reddehase MJ, Riddell SR, Busch DH. TCR-ligand koff rate correlates with the protective capacity of antigen-specific CD8+ T cells for adoptive transfer. Sci Transl Med. 2013.5:192ra87. doi: 10.1126/scitranslmed.3005958.
Chopra M, Biehl M, Steinfatt T, Brandl A, Kums J, Amich J, Vaeth M, Kuen J, Holtappels R, Podlech J, Mottok A, Kraus S, Jordán-Garrote AL, Bäuerlein CA, Brede C, Ribechini E, Fick A, Seher A, Polz J, Ottmüller KJ, Baker J, Nishikii H, Ritz M, Mattenheimer K, Schwinn S, Winter T, Schäfer V, Krappmann S, Einsele H, Müller TD, Reddehase MJ, Lutz MB, Männel DN, Berberich-Siebelt F, Wajant H, Beilhack A. Exogenous TNFR2 activation protects from acute GvHD via host T reg cell expansion. J Exp Med. 2016. 213:1881-900. doi: 10.1084/jem.20151563.
For more publications see here
- Members
- Techniques
- Literature