Interdisciplinary Infection Medicine Mainz (IIM)
Speaker: Dr. Ingo Sagoschen (Center for Cardiology)
Last meeting:
Tuesday June 1st, 2021 - 4:45pm - online
Tuesday June 1st, 2021 - 4:45pm - online
(new appointments TBA)
Aims/Content
Our aim is to establish and develop Infection Medicine practically with all its facets. This includes an adequate microbiological diagnostic, appropriate practiced infection prevention and a rational therapy with anti-infective substances.The representatives of the following institutions of the University Medical Center are joining the “Interdisciplinary Infection Medicine Mainz”:
- Institute of Medical Microbiology and Hygiene
- Institute of Virology
- Pharmacy of the University Medical Center
- Department of Internal Medicine I
- Department of Cardiology
- Department of Internal Medicine III
- Department of Pediatrics
- Department of Obstetrics and Gynecology
- Department of Neurology
- Infectiological Board (Info: Dr. Ekkehard Siegel)
- Guidelines "Kalkulierte Antibiotikatherapie 4.1" at the University Medical Center Mainz
(Info: Dr. Ingo Sagoschen)- for outpatient clinics, normal and intensiv care units [pocket size, internally via printing department (Best.-Nr. UKM 11-198)]
(PDF version available on the pharmacy's website intranet) - for intensive care units (DIN A3 poster) (current version 2023)
(PDF version available on the pharmacy's webiste intranet)
Further wishes/feedback welcome: antibiotikaempfehlung@unimedizin-mainz.de - for outpatient clinics, normal and intensiv care units [pocket size, internally via printing department (Best.-Nr. UKM 11-198)]
- "Führerschein Infektionsmedizin" - after the official start in July 2017, this externally open advanced training course on the basic principles of modern ABS-based infectious disease medicine now takes place quarterly (Info: Dr. Ingo Sagoschen, Dr. Bettina Siegrist, Dr. Moritz Brandstetter).
- Case-based training "Ansteckend" - once a semester, infection medicine can be learned through case presentations: interdisciplinary and concrete.
- Establishment of the center “Infektionsmedizin nach DGI”
Since June 2019 it is official: the Deutsche Gesellschaft für Infektiologie (DGI) approved us as DGI-center (DGIZ) for the next five years. This includes: I. Medical Clinic and Polyclinic, III. Medical Clinic and Polyclinic, Center for Cardiology, Institute of Virology and Institute of Medical Microbiology and Hygiene.
- Infectiological consultation service (Info: Dr. Martin Dennebaum )
Currently, the conditions have been adjusted: Via the telephone center of the University Medical Center Mainz, you can reach the respective responsible colleague of the participating institutions. Contacting via fax or email is possible, too:
Fax: +496131 17- 47 5529 - Training Series Infectiology (Info: PD. Dr. Martin Sprinzl)
In regular, mostly monthly intervals, 30-minute advanced training courses on infectious medicine topics are held; the curriculum, which is designed for a period of two years, covers all relevant areas of infectiology. Advanced training points for the medical association and DGI are applied for.
- Antibiotic-Stewardship-Program (Info: Dr. Ingo Sagoschen)
- ABS-courses: Many employees of the "Interdisciplinary Infection Medicine Mainz" design all 5 modules of the ABS courses in cooperation with the Academy for Medical Training in Mainz according to the curriculum of the BAEK. In this way, we actively contribute to the possibility of being trained to become an ABS-assigned physician and ABS specialist in Mainz. The modules for the ABS-assigned physician take place once a year in autumn and the supplementary modules for the ABS Expert in late spring (May). (Info: Dr. Ingo Sagoschen)
- Therapeutic Drug-Monitoring for established antibiotics (Info: Dr. Ingo Sagoschen)
- Coordination of clinical-infectiological studies (Info: contact person TBA)
- Establishment and regular amendment of diagnostic and therapeutic standards in tropical-, travel medicine and parasitology questions. (Info: Dr. Martin Dennebaum)
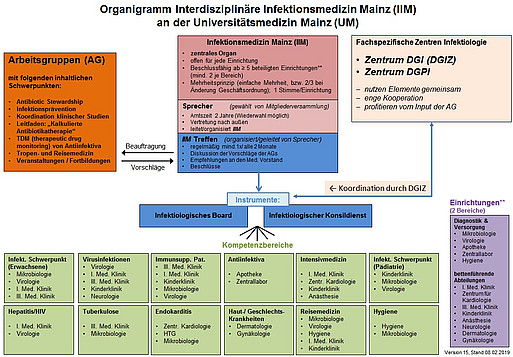
Structure and organigram of the Interdisciplinary Infection Medicine Mainz
Information on penicillin allergy
Penicillin allergyUp to 10% of the population claim to have a penicillin allergy. In fact, 85-90% of all patients with anamnestic penicillin allergy tolerate penicillins because they are not or no longer allergic.
Consequences of a supposed penicillin allergy are avoidance of beta-lactam antibiotics such as penicillins and cephalosporins. Alternative anti-infectives are often less effective, have more side effects, induce more resistance and cause higher costs.
Patients, who claim to have a penicillin allergy, are for example twice as likely to receive vancomycin and three times as likely to receive fluoroquinolones. They have 23% more C. difficile infections, 14% more methicillin-resistant staphylococcus aureus (MRSA) infections and 30% more evidence of vancomycin-resistant enterococci (AER).
Therefore, a suspected penicillin allergy should always be clarified and not be taken over uncritically. In addition to in vitro tests, skin tests and oral provocation are available for testing.
A penicillin allergy does not has to last a lifetime: About 50% of patients with IgE-mediated penicillin allergy lose sensitivity 5 years after the last reaction (about 80% after 10 years!).
97-98% of patients with penicillin allergy confirmed by skin testing tolerate cephalosporins!
Patients, who urgently need to be treated with a beta-lactam antibiotic, a desensitization can be carried out at short notice.
Indication: patients with confirmed (positive skin test or in vitro test) or urgently suspected LgE-mediated immediate reaction to penicillin AND for whom there are no comparably effective alternatives.
Contraindication: Anamnesis of Stevens-Johnson syndrome, exfoliative dermatitis or erythroderma. A desensitization temporarily alters the immune response to the antibiotic in the sense of short-term tolerance, which enables a safe medication (if taken continuously!).
Sources:
- Park M, Markus P, Matesic D, Li JT. Safety and effectiveness of a preoperative allergy clinic in decreasing vancomycin use in patients with a history of penicillin allergy. Ann Allergy Asthma Immunol 2006; 97:681.
- Macy E, Contreras R. Health care use and serious infection prevalence associated with penicillin "allergy" in hospitalized patients: A cohort study. J Allergy Clin Immunol 2014; 133:790.
- Lee CE, Zembower TR, Fotis MA, et al. The incidence of antimicrobial allergies in hospitalized patients: implications regarding prescribing patterns and emerging bacterial resistance. Arch Intern Med 2000; 160:2819.
- Borish L, Tamir R, Rosenwasser LJ. Intravenous desensitization to beta-lactam antibiotics. J Allergy Clin Immunol 1987; 80:314.
- Daulat S, Solensky R, Earl HS, et al. Safety of cephalosporin administration to patients with histories of penicillin allergy. J Allergy Clin Immunol 2004; 113:1220.
Current and relevant literature from the world of infection medicine:
- S3-Guidelines "Strategies to ensure rational use of antibiotics in hospitals" (AWMF website http://www.awmf.org )
- Guidelines for the prevention of surgical site infection_November2016(PDF 1,5 MB)
- Targeted versus universal decolonization to prevent ICU infection_Huang_NEJM2013
- Daptomycin - current discussion on application areas and dosage (website of the medicines commission of the German medical profession)
COVID-19 diagnostics: SARS-CoV-2
In consultation with our colleagues at the virological institute, we have compiled information on the diagnosis of infections when COVID-19 is suspected.(PDF 721,4 KB)Diagnostics are currently performed at the Institute of Virology of the University Medical Center Mainz.
The Robert Koch Institute has developed an action plan to clarify a suspicious case.
Further information can be found on the websites of the Robert Koch-Institute (RKI) and the WHO.
The Robert Koch Institute has developed an action plan to clarify a suspicious case.
Further information can be found on the websites of the Robert Koch-Institute (RKI) and the WHO.